Abstract
Introduction: Polycythemia vera (PV) is a classical myeloproliferative neoplasm characterized by the overproduction of mature red blood cells leading to an increased risk of thrombosis. Maintenance of hematocrit below 45% using phlebotomy improves rate of cardiovascular death and major thrombosis and is recommended for all PV patients. For high risk patients (> 60 years and/or with thrombosis history) cytoreductive therapy is recommended, with hydroxyurea (HU) being most commonly used among older PV patients. Little is known about the patterns of care and the impact of phlebotomy and HU on the outcomes of PV patients in the real-world setting.
Methods: We conducted a retrospective cohort study of older adults (aged 66-99 years) diagnosed with PV (International Classification of Diseases for Oncology, 3rd edition, code 9950) in 2007-2011 and included in the Surveillance, Epidemiology, and End Results (SEER)-Medicare linked database. Patients were required to have: 1) continuous enrollment in Medicare Parts A and B from one year before PV diagnosis through death or end of study (12/31/2012), whichever came first; and 2) continuous Part D coverage from diagnosis to end of follow-up to capture HU use. HU users were restricted to those who had more than two HU prescription claims. Predictors of receiving phlebotomy or HU were evaluated using multivariate logistic regression models. Thrombotic events were defined as the first occurrence of venous thrombosis, or arterial thrombosis, or sudden death after diagnosis. Multivariate Cox models were used to assess the impact of phlebotomy and HU on two outcomes measured from the time of diagnosis, including overall survival and time to the above mentioned thrombotic events, adjusting for patient age at diagnosis, sex, race, Part D low income subsidy (LIS, a proxy marker for reduced out-of-pocket cost sharing, and lower socioeconomic status), influenza vaccination 12 months prior to diagnosis (an indicator for health care access), disability status (a claims-based proxy for poor performance status), modified Elixhauser comorbidity score (the original comorbidity score excluding cardiovascular conditions), and pre-existing cardiovascular conditions. Phlebotomy and HU were treated as time-dependent variables.
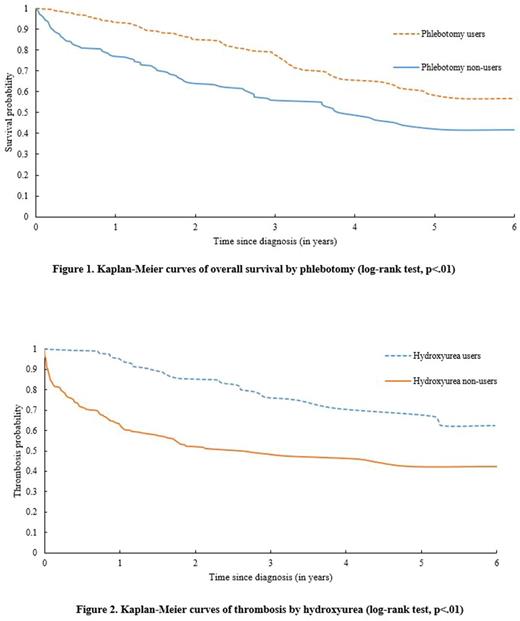
Results: A total of 482 PV patients with a mean age of 77.7 years were identified. The majority of patients were female (55.6%) and white (90.0%). During the study period, 376 (78.0%) received phlebotomy and/or HU. Among them, 136 (36.2%) patients underwent therapeutic phlebotomy only, 95 (25.2%) received HU only, and 145 (38.6%) received both phlebotomy and HU. On multivariable regression, patients with increasing age (p=.01) and non-white (p=.01) were less likely to get phlebotomy; whereas patients who were male (p<.01), lacked influenza vaccination 12 months before diagnosis (p<.01), and who were without LIS (p=.01) were less likely to receive HU. After a median follow-up of 2.75 years, 28.8% (n=81) phlebotomy users and 46.8% (n=94) phlebotomy non-users died. The median survival for phlebotomy non-users was 3.81 years, while for phlebotomy users it was not reached (log-rank test, p<.01, Figure 1). In the multivariate Cox model, receipt of phlebotomy was significantly associated with a lower risk of death (hazard ratio [HR]=0.71, 95% confidence interval [CI]: 0.52-0.96, p=.03). While HU use was not associated with overall survival (users vs. non-users: HR=0.85, 95% CI:0.62-1.16, p=.30), HU users were less likely to experience a thrombotic event after PV diagnosis (21.4% vs. 46.5%, p<.01). Median time to develop thrombosis for HU non-users was 2.64 years while for HU users it was significantly longer (not reached, log-rank test, p<.01, Figure 2). HU use remained associated with a lower risk of thrombosis after PV diagnosis on multivariable Cox regression (HR=0.47, 95% CI: 0.33-0.68, p<.01). On similar models, phlebotomy use was not strongly associated with the development of thrombosis.
Conclusions: In this population-based study reflecting general clinical practice, phlebotomy use was associated with improved overall survival among older adults with PV while HU-treated patients had decreased risk of thrombosis. Both treatment modalities were underused in this high-risk PV population.
Podoltsev: Incyte: Consultancy; CTI biopharma/Baxalta: Consultancy; Ariad: Consultancy; Alexion: Consultancy. Zeidan: Takeda: Speakers Bureau; Otsuka: Consultancy; AbbVie, Otsuka, Pfizer, Gilead, Celgene, Ariad, Incyte: Consultancy, Honoraria. Huntington: Celgene: Consultancy, Other: Travel; Janssen: Consultancy; Pharmacyclics: Honoraria. Ma: Incyte Corp.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal